You wake up stiff.
Your rings feel tight.
Your joints ache more than they should.
Your face looks puffier than it used to.
Your body feels… inflamed.
Not injured.
Not sick in the traditional sense.
Just swollen, reactive, uncomfortable in your own skin.
And when labs are checked, you may hear:
“Everything looks normal.”
But your body still feels like it won’t settle.
This is the pattern I refer to as:
The Inflammation Loop.
And it’s far more common than most women realize.
What Is the Inflammation Loop?
Inflammation isn’t inherently bad.
It’s a protective response — your body’s way of repairing, defending, and adapting.
But when inflammation becomes chronic and low-grade, it stops being helpful and starts becoming disruptive.
This can show up as:
joint pain
muscle stiffness
fluid retention
skin changes
digestive discomfort
fatigue
weight resistance
You don’t feel acutely ill — you feel persistently inflamed.
Why Inflammation Becomes “Sticky”
Inflammation rarely exists in isolation.
It’s influenced by multiple overlapping inputs:
stress physiology
blood sugar instability
nutrient deficiencies
immune activation
recovery capacity
When these factors layer, inflammation becomes self-reinforcing — a loop instead of a temporary response.
CRP: The Inflammation Marker Most People Know
C-reactive protein (CRP) is often used as a general inflammation marker.
Elevated CRP can reflect:
systemic inflammation
immune activation
metabolic stress
injury or infection
But here’s where interpretation matters:
CRP may sit “in range” — while still reflecting enough inflammatory load to affect how you feel.
Again: pattern over thresholds.
Ferritin: More Than Iron Storage
Ferritin is typically viewed through an anemia lens.
But it also functions as an acute-phase reactant — meaning it rises in response to inflammation.
So ferritin can reflect:
iron storage
inflammatory signaling
immune activation
Low ferritin can impair energy and recovery.
High ferritin can signal inflammatory load.
Context determines meaning.
Vitamin D: Immune Modulator, Not Just a Vitamin
Vitamin D influences:
immune regulation
inflammatory response
mood
recovery
musculoskeletal health
Low or low-normal vitamin D can contribute to:
pain sensitivity
fatigue
immune dysregulation
inflammatory persistence
It doesn’t create inflammation alone — but it affects how well the body resolves it.
Blood Sugar and Inflammation
Glucose instability fuels inflammatory signaling.
Frequent spikes and crashes can:
Even when A1c is normal, daily glucose swings can quietly sustain inflammatory patterns.
Why the Body Feels Puffy, Achy, and Reactive
When inflammation is chronically activated, women often describe:
This isn’t imagination.
It’s physiology under strain.
Why Isolated Fixes Rarely Work
This is where frustration builds.
Women try:
anti-inflammatory diets
supplements
detox protocols
elimination plans
Some help temporarily — but symptoms return.
Because inflammation loops are driven by:
stress load
metabolic signaling
nutrient sufficiency
immune balance
You can’t solve a loop by pulling one lever.
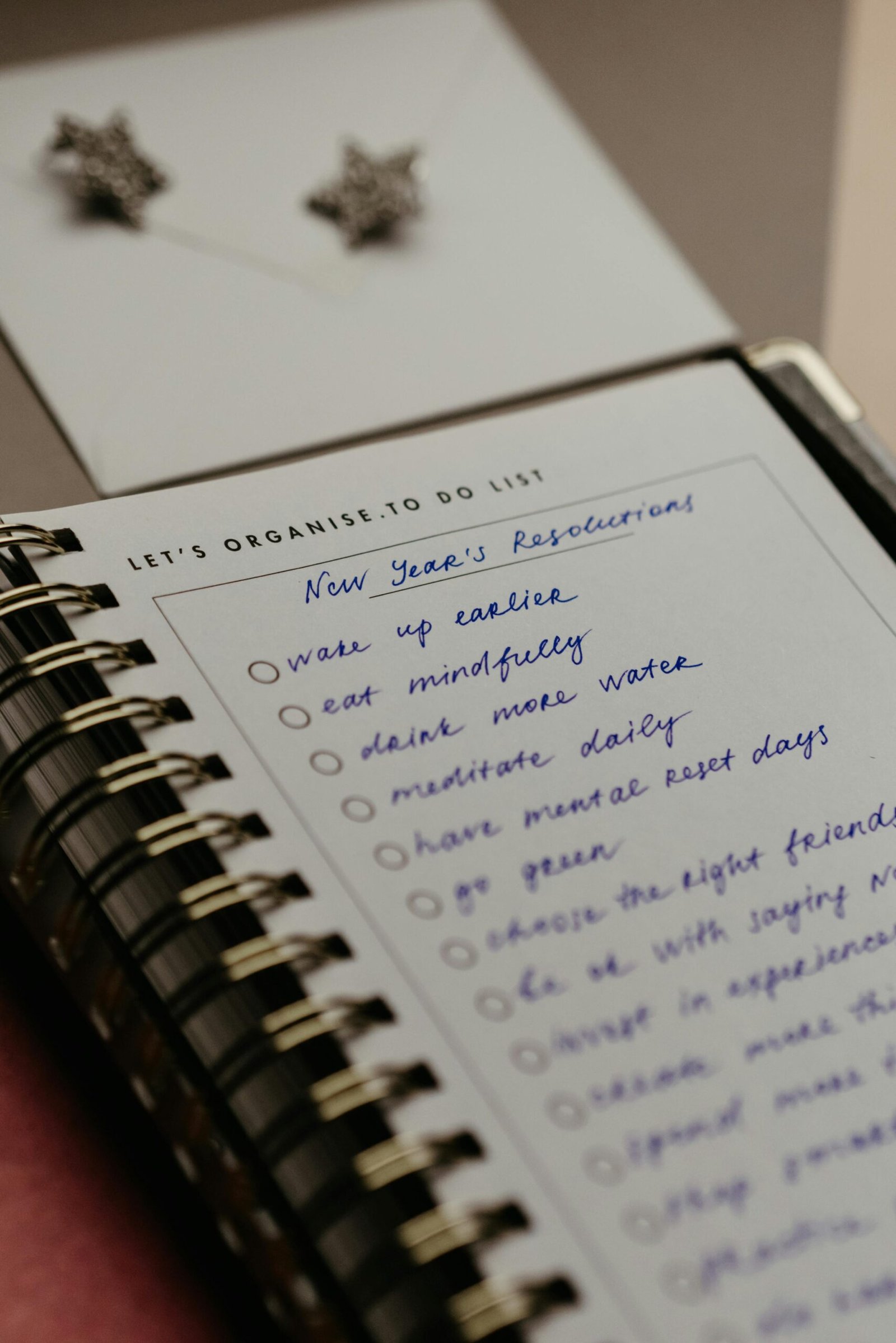
The Reframe That Changes the Approach
Inflammation isn’t something to “attack.”
It’s something to understand.
Your body isn’t inflamed because it’s malfunctioning.
It’s inflamed because it’s responding — to stress, instability, deficiency, or overload.
When you address the pattern, inflammation often softens naturally.
Signs You May Be in an Inflammation Loop
You might recognize yourself if you:
wake stiff or swollen
feel puffy despite clean eating
experience joint discomfort without injury
retain fluid easily
struggle with inflammatory weight
feel sore longer than you should
These are signals — not flaws.
Why This Pattern Is Hard to Navigate Alone
Most inflammation advice is protocol-based:
remove foods
add supplements
follow a plan
But inflammation patterns require context:
stress physiology
blood sugar regulation
nutrient sufficiency
immune balance
Without that lens, women end up cycling fixes instead of resolving patterns.
If You Recognize Yourself Here
If you’ve ever felt like your body just won’t calm down — no matter how clean you eat or how well you take care of yourself — you’re not alone.
And you’re not imagining it.
This is exactly the kind of pattern we explore in clarity calls — connecting inflammation markers, metabolic patterns, stress load, and lifestyle factors.
👉 If this made you realize your body isn’t broken — it’s responding, I offer free 60-minute clarity calls to help you connect the dots and figure out what actually matters for your body.
Want to Learn More?
If this pattern feels familiar, these articles may help you understand the bigger picture:
Why Your Labs Are “Normal” — But You Still Don’t Feel Well
If you’ve been told everything looks fine but your body feels anything but, this foundational article explains why symptoms often show up before labs do.
The Wired-Tired Pattern: When Cortisol, Blood Sugar, and Burnout Overlap
How stress hormones and metabolic instability create exhaustion, inflammation, and nervous system overload.
Weight Loss Resistance: When Thyroid, Insulin, and Stress Work Against You
A deeper look at how inflammation, metabolic signaling, and hormonal patterns influence fat storage and progress plateaus.
The Connection Between Cortisol, Sleep, and Weight Gain
How chronic stress reshapes recovery, inflammation, and metabolic health — even when lifestyle habits look supportive.